Sweat, like blood, can tell us a lot about a person’s health. And conveniently, it’s a lot less invasive to collect. This is the premise behind the wearable sweat sensors developed by Wei Gao, assistant professor of medical engineering, Heritage Medical Research Institute Investigator, and Ronald and JoAnne Willens Scholar.
Over the past five years, Gao has steadily added features to his wearables, making them capable of reading out levels of salts, sugars, uric acid, amino acids, and vitamins as well as more complex molecules like C-reactive protein that can provide timely assessment of certain health risks. Most recently, in collaboration with Martin Kaltenbrunner’s group at Johannes Kepler University Linz in Austria, Gao has powered these wearable biosensors with a flexible solar cell.
The solar cell used by Gao’s lab is made of perovskite crystal, a material that shares the chemical structure first found in the mineral calcium titanium oxide. Perovskite has captured the attention of solar cell developers for several reasons:
First, it is cheaper to manufacture than silicon (the primary material used in solar cells since the 1950s), which must be highly purified through multiple processes.
Second, perovskite is as much as 1,000 times thinner than silicon solar cell layers, making them “quasi-2D” in Gao’s terms.
Third, perovskite can be tuned to the spectra of different lighting, from outdoor sunlight to various forms of indoor lighting.
Finally, and most enticingly for pioneers of solar energy, perovskite solar cells achieve a higher power conversion efficiency (PCE) than silicon, which means they can convert a greater proportion of the light they receive into usable electricity.
Silicon solar cells have reached PCE levels that range from 26–27 percent, though in regular use the range hovers between 18 and 22 percent. By contrast, the flexible perovskite solar cell (FPSC) on Gao’s wearable sweat sensor has a record-breaking PCE exceeding 31 percent under indoor light illumination.
“We don’t want to only use strong sunlight to power our wearables,” Gao explains. “We care about more real-life conditions, including normal office and home lighting. Many solar cells have high efficiency in strong sunlight but not in weak indoor lighting conditions.” The FPSC on the sweat sensor is particularly well suited to indoor lighting, says Gao, as “the spectral response of the FPSC matches well with the common indoor lighting emission spectrum.”
Previous iterations of Gao’s wearable sweat sensors were powered by lithium-ion batteries that were bulky and had to be recharged with an external source of electricity. The search for a lighter, more renewable source of electricity to power these high-demand devices led Gao’s lab to try using silicon solar cells, which they found to be too rigid, inefficient, and reliant on strong lighting conditions.
They also experimented with harvesting energy from the chemicals in human sweat (a readily available biofuel) and body motion but found these were too unstable or required too much effort on the part of the wearer.
Use of a FPSC has allowed Gao to create sweat sensors that can be worn for 12 hours a day, providing continuous monitoring of pH, salt, glucose, and temperature, and periodic monitoring (every five to 10 minutes) of sweat rate. All of this is accomplished without batteries or a specially dedicated light source. Furthermore, as the power source has become lighter and less cumbersome, the wearable has room for additional detectors to monitor a greater number of biomarkers simultaneously.
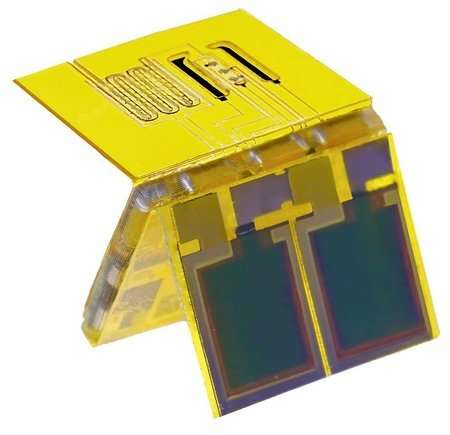
This new wearable sweat sensor, like its predecessors, is assembled in an origami-like fashion, with individual layers dedicated to different processes. The sensor has four principal interacting components. The first is dedicated to power management—disbursing the electricity harvested by the solar cell. The second enables iontophoresis, the induction of sweating without any exercise or exposure to high heat required on the part of its wearer.
In Gao’s study, iontophoresis was performed every three hours to ensure that enough sweat was available to continuously monitor the biomarkers under observation. The third enables the electrochemical measurement of various substances in the sweat. The fourth manages data processing and wireless communication, which allows the sensor to interface with a cellphone app to display the ongoing results of the sensor’s monitoring.
Fully assembled, the sensor measures 20 x 27 x 4 millimeters, and it can handle the mechanical stress associated with being worn on the body. “Most of the elements of the sweat sensor, such as the electronics and the FPSC, are reusable,” Gao adds. “The only exception is the sensor patch, which is disposable, and it can be mass produced at a low cost using inkjet printing.” These sensor patches can also be customized according to what substances the user wishes to measure in their body.
As these solar-powered sweat sensors are put to use, they will be able to measure far more than any fitness or health tracker currently does. For example, they can be used for diabetes management (studies have shown that glucose in sweat is closely matched to glucose in the blood) and for the detection of a range of conditions such as heart disease, cystic fibrosis, and gout.
Because they are noninvasive and can perform multiple measurements over short periods of time, these sensors can discern an individual’s baseline for substances such as cortisol, hormones, or the metabolites of various nutrients and medicines.
Once the baseline levels for such substances are known, future deviations from these will provide a more effective means of diagnosis than a single blood draw ever could. And because the sensors are relatively inexpensive, the hope is that they can be an excellent diagnostic tool across the globe, including in developing countries.